Nov 7, 2024
Is the U.S. Mental Healthcare System Broken?
Some long-term solutions and one that’s a little faster
Let’s just start with the obvious: the United States is facing a mental health crisis. We’ve been talking about it for many years now. For more than a decade, rates of depression, anxiety, and other psychological disorders have been rising, especially among young people.
This has been thoroughly documented in countless studies. Well-known researchers like Jonathan Haidt and many others have written best-selling books and have many different media channels for these discussions.
While there are some denialists, it would seem they are in the small minority, cherry-pick their data, and/or have a clear motivation (akin to how the tobacco companies had a vested interest in denying tobacco was harmful to one's health). We are not here to get into these issues in this article. We are merely setting the stage for what seems as clear as any “reality” we’re experiencing in the cultural collective.
There is so much data now it’s almost hard to know what to choose to illustrate the issue on a broad scale, but let’s just use this one example:
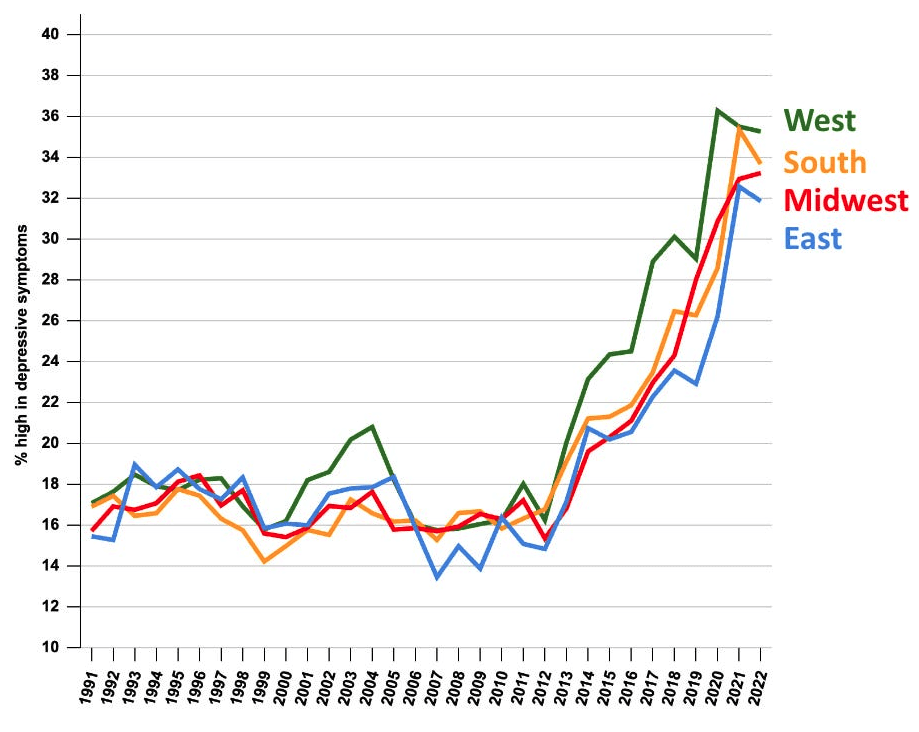
Percent of U.S. teens with high depressive symptoms, by region, 1991–2022. Source: Monitoring the Future.
This suggests a national cause for the increase rather than something more regional such as the opioid crisis or economic shifts in the Midwest.In light of how rapid and acute the levels of stress and anxiety have risen, it should probably come as no surprise that our mental healthcare system remains fragmented, underfunded, and inaccessible for far too many Americans.
In a 2022 report, the American Psychological Association (APA) found that over 160 million adults live in federally-designated mental health professional shortage areas. That’s nearly half the population. Therapists, psychiatrists, and other providers are simply stretched too thin to meet the surging demand. And for those who can access care, the costs are often prohibitive — a single therapy session can cost hundreds of dollars out-of-pocket, putting treatment out of reach for many.“
The pandemic has only exacerbated long-standing challenges in our mental healthcare system,” says Dr. Sarah Martinez, a clinical psychologist at the University of California, San Francisco. “We’re seeing skyrocketing rates of depression, anxiety, and other issues, but the system was already overburdened and underfunded before COVID-19 hit.”
Indeed, a 2021 study in JAMA Psychiatry found that the use of mental health treatment services increased by over 700% from 2019 to 2020, with the steepest rise among young adults. Yet, data from the Substance Abuse and Mental Health Services Administration shows that nearly 60% of adults with a mental illness received no treatment at all in 2020.
Experts point to a perfect storm of systemic barriers limiting access to quality mental healthcare:
Insurance Coverage
Despite the passage of the Mental Health Parity Act in 2008, which requires insurers to cover mental health services on par with physical health, many plans still impose stricter limits. A 2021 report by the Congressional Budget Office found that patients faced significantly higher out-of-pocket costs for mental health visits compared to primary care. This financial burden causes many to forgo necessary treatment.
Workforce Shortages
Even for those with adequate insurance, finding an available provider can be a challenge. A 2022 report by the Health Resources and Services Administration projected a shortfall of over 13,700 psychiatrists by 2025. The pipeline of mental health professionals simply cannot keep up with surging demand.
“We’re losing providers faster than we can train new ones,” says Dr. John Wilkins, chair of psychiatry at Ohio State University. “Burnout is rampant, with many clinicians leaving the field due to the immense stress and administrative burdens.”
Disparities in Access
Marginalized communities face some of the starkest barriers. Studies show that racial and ethnic minorities, LGBTQ+ individuals, and those with lower incomes are less likely to receive adequate mental healthcare. Factors like lack of culturally competent providers, transportation issues, and language barriers only exacerbate the disparities.
A Byzantine System
The fragmentation of the U.S. healthcare system compounds access challenges. Mental health and physical health services are often siloed, with poor coordination between providers. This makes it difficult for patients to navigate the system and receive comprehensive, integrated care.“We need to move towards a more holistic, whole-person approach,” argues Dr. Martinez. "Right now, the system is far too compartmentalized, with mental health treatment existing separate from primary care. That has to change.”
So, what’s the path forward?
Let’s start with what we’ve been hearing from experts and advocates over the years (if not decades) about suggested systemic reforms.
And before you roll your eyes, just give their ideas a chance, and remember that these people are at least trying to come up with solutions.
Expand Insurance Coverage and Reimbursement
Policymakers should strengthen mental health parity laws, increase Medicaid funding for behavioral health services, and incentivize insurers to provide more robust, affordable coverage. This could significantly improve access and reduce out-of-pocket costs.
Grow the Mental Health Workforce
Initiatives to recruit, train, and retain more mental health providers — from psychiatric nurses to clinical social workers — are crucial. This could involve loan forgiveness programs, enhanced training pipelines, and better compensation to address burnout.
Integrate Care and Address Social Determinants
Integrating mental health services into primary care settings, as well as addressing social factors like housing, employment, and education, can help provide more holistic, person-centered care. Community-based programs that connect individuals to a range of support services are also important.
Increase Funding and Infrastructure
Significantly more public and private investment is needed to build out mental healthcare infrastructure, from inpatient facilities to telehealth platforms. Policymakers should earmark funding for everything from crisis hotlines to suicide prevention programs.
Prioritize Prevention and Early Intervention
Rather than focusing solely on acute treatment, the system should place greater emphasis on mental health promotion, resilience-building, and early intervention — especially for youth. This can reduce long-term costs and improve outcomes.
“We know what works to improve mental healthcare access and quality,” says Dr. Wilkins. “The challenge is marshaling the political will and resources to actually implement these solutions at scale. But given the immense human and economic toll of this crisis, we have no choice but to act.”
While we don’t disagree with any of these well-intentioned ideas per se, it’s not as if these haven’t long since been on the table. Further, these are multivalent solutions, which even with huge sources of funding and good intentions will take many years to make significant change. As for the latter idea of prevention, well, yeah, who doesn’t agree?
Massive Final Takeaway and a Ray of Sunshine
And that leads us to our modest proposal. We’re not saying that we’re single-handedly solving the mental healthcare crisis. Not by a long shot. But our carefully curated AI coach, EMMA, does offer a ray of sunshine that addresses most of the issues related to accessibility, cost, and the idea of prevention in a single shot.
To be clear, EMMA does not “diagnose.” It does not take the place of anything like a clinical opinion for very real chemical and physical conditions.
But EMMA does do what any good coach does. EMMA listens, asks questions, offers guidance and partnership. And then, EMMA is positioned to hold you accountable and even challenge you when you don’t always follow through with your goals. EMMA provides clarity for people who need it.
Of course, as with any coach, you have to recognize you need some support and assistance. You need the intention in the first place.
But with that intention, we see cause for optimism. The world of AI doesn’t have to be a disconnected dystopian future full of fake plastic trees and metaverses. No, AI can serve humanity for more than just whipping out a fast and generic term paper, and we’re seeing it right now in the present moment.
While we push for major reforms in the mental health industry that will take years or even decades to realize, there are millions of lives that can be improved right now in real time. And for those going through acute burnout and stress and anxiety right now, that is most welcome news.





